

Burger menu icon
Caret down icon
Thick caret down icon
Thick close icon
Filled arrow up icon
Thin left arrow icon
Thin right arrow icon
By continuing on our website, you agree to our use of the cookie for statistical and personalization purpose. Learn More
Our Scorecard ranks every state’s health care system based on how well it provides high-quality, accessible, and equitable health care. Read the report to see health care rankings by state.
International Health Care System Profiles


Multipayer, mixed insurance system: MediShield Life, universal basic health insurance for catastrophic expenses; MediSave, mandatory individual savings account for hospital and selected outpatient expenses; MediFund, safety net for low-income citizens; subsidies provided to all for care at public facilities and accredited private primary care facilities.
General tax revenue
Secondary Health Insurance
Coverage for private hospitals or care in private wards in public hospitals. 68% have an Integrated Shield Plan to supplement MediShield coverage. Additional forms of for-profit insurance, including employer coverage.
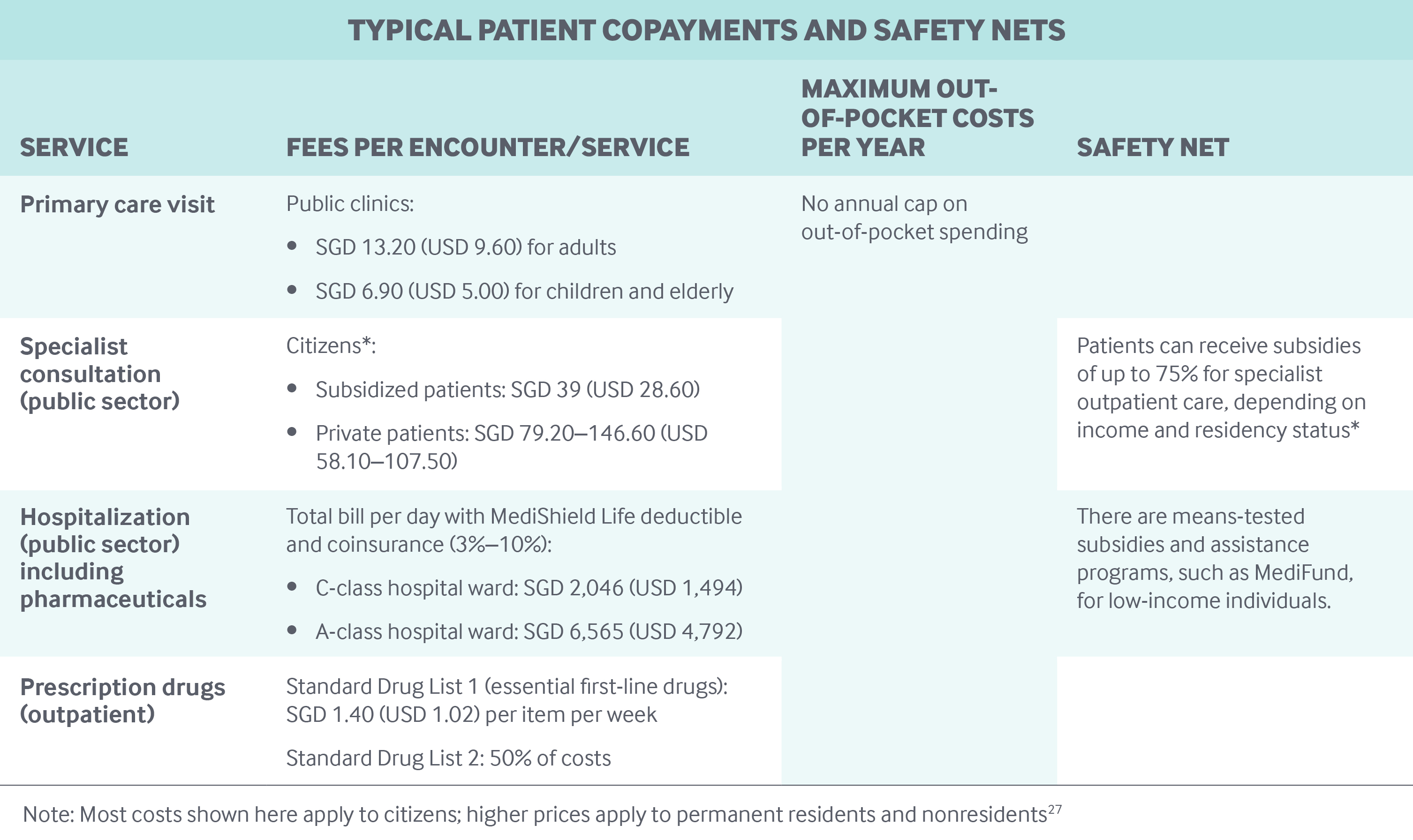
Patient Cost-Sharing close icon Physician VisitsPrimary care: Adults in public clinics: SGD 13.20 (USD 9.60) per consultation.
Specialists: Subsidized patients: SGD 39 (USD 28.60). Private patients: SGD 79.20–146.60 (USD 58.10–107.50) for consultations in public facilities.
Hospital Inpatient Care
MediShield Life: Deductible of (SGD 1,500–3,000 (USD 1,095–2190) plus 3%–10% coinsurance. Total cost varies by ward type.
Prescription Drugs
Essential/standard drugs: Up to 50% of costs. Additional subsidy based on income from Medication Assistance Fund for high-cost nonstandard drugs.
Caps on Cost-Sharing
Safety Nets
Lower primary care copays for children and elderly. Subsidies for hospital care based on ward class, income, and residency status and for specialist outpatient care based on residency status. MediFund is safety net for low-income people. Community Health Assist Scheme provides income-based subsidies for citizens towards care at private GP and dental clinics. Government supplements/top-ups to MediSave accounts of low-income people, elderly, newborns.
Providers close icon Primary CareMostly private providers, paid mostly FFS. No formal gatekeeping but lower patient cost-sharing with referrals in public system and accredited private providers. Patient registration not required.
Mainly public, remainder mostly for-profit. Paid through case-based payments (DRGs) within global budget.
Medical Schools close icon OwnershipTuition Fees
Heavily subsidized. Annual fees after subsidy: SGD 29,000–33,000 (USD 21,000– 24,000) for nationals for five-year undergraduate program; SGD 47,000 (USD 34,000) for four-year graduate program.
By Lee Chien Earn, National University of Singapore
Singapore has achieved universal health coverage through a mixed financing system. The country’s public statutory insurance system, MediShield Life, covers large bills arising from hospital care and certain outpatient treatments. Patients pay premiums, deductibles, co-insurance, and any costs above the claim limit. MediShield Life generally does not cover primary care or outpatient specialist care and prescription drugs. MediShield Life is complemented by government subsidies, as well as a compulsory medical savings account called MediSave, which can help residents pay for inpatient care and selected outpatient services. In addition, individuals can purchase supplemental private health insurance or get it through an employer. The national government is fully responsible for the health system.
Singapore’s health care financing system is underpinned by the belief that all stakeholders share responsibility for attaining sustainable universal health coverage. Singapore has a multipayer health care financing framework, where a single treatment episode might be covered by multiple schemes and payers, often overlapping. The system, known as the 3Ms, comprises the following programs:
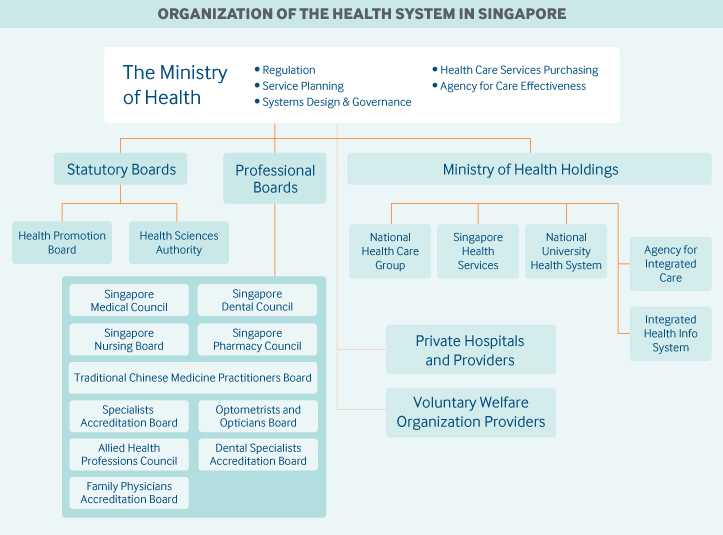
Role of government: The Ministry of Health’s mission is to promote good health and reduce illness, ensure access to good and affordable health care, and pursue medical excellence. The Ministry of Health is responsible for regulating the public health system and the health care system overall. 2
The government relies on competition and market forces to improve service and raise efficiency but intervenes directly when the market fails to keep health care costs down. 3 For example, the Ministry of Health performs workforce planning to determine the number of health care professionals required, coordinates the training capacity, and dictates land availability for hospital and other health care facility development. 4 The ministry also ensures that longer-term population needs are met through sustainable investment, especially in preventive and community-based care. 5
The Ministry of Health has centralized certain functions to prevent fragmentation and to encourage economies of scale. National organizations with important functions include the following:
Role of public health insurance: Singapore’s national health expenditures stood at 4.47 percent of GDP in 2016. 7 Between 2009 and 2016, the government’s share of health expenditures increased from about 32 percent to 41 percent due to increased public subsidies, which are intended to help reduce out-of-pocket costs. 8 Correspondingly, the out-of-pocket share of health expenditures fell from 43 percent to 31 percent. Singapore’s average annual health care inflation was 2.6 percent, compared to 2.3 percent for all goods and services, between 2007 and 2017. 9
MediShield Life premiums are subsidized by the government on the basis of income. In addition, working-age persons pay higher premiums so that older residents can have lower premium increases. These features have helped to keep annual premiums affordable, ranging from SGD 98 (USD 72) 10 for low-income Singaporeans under age 20 to SGD 1,530 (USD 1,117) for high-income residents over age 90. 11 To ease the transition from the old MediShield scheme’s lower premiums (with its age cut-off and exclusion of those with preexisting illnesses) to the higher premiums of MediShield Life, which provides lifelong coverage, beneficiaries with serious preexisting conditions pay 30 percent higher premiums for the first 10 years, after which they pay the same standard premium as their low-risk counterparts. 12 During the first five years of MediShield Life, the government cushioned the impact of bringing beneficiaries with preexisting conditions into the scheme by absorbing about 75 percent of the costs, which was approximately SGD 850 million (USD 621 million). 13
The government provides various other subsidies to help make care more affordable:
In addition, the Community Health Assist Scheme, for lower- to middle-income citizens, provides subsidies that can be used at private general practitioner (GP) and dental clinics. About 1.2 million Singaporeans are in the scheme, and they receive subsidized care at more than 1,000 GPs and 700 dental clinics. 15 In 2018, the government disbursed about SGD 152 million (USD 111 million) in subsidies under the Community Health Assist Scheme to about 630,000 Singaporeans. 16
Government health care subsidies are funded from general taxation and are based on the principles of fiscal balance and affordability.
The government has also introduced measures to supplement Singaporeans’ MediSave accounts. For example, lower-income workers receive top-ups to help them save for their retirement health care needs. 17 The government also provides annual top-ups to the MediSave accounts of eligible elderly people and gives newborns a MediSave grant of SGD 4,000 (USD 2,940) to defray part of their parents’ infant care expenses.
Role of private health insurance: Patients who wish to obtain additional coverage for private hospitals or care in private wards in public hospitals can purchase private insurance. The most common coverage is through Integrated Shield Plans, which ride on MediShield Life and are available only to citizens and permanents residents with MediShield Life. As of 2017, 68 percent of citizens and permanent residents had one of these plans. 18 In contrast to the standard benefits of MediShield Life, different Integrated Shield Plans offer different benefits. Premiums for these plans can be paid for using MediSave, subject to various limits and regulations. 19
Integrated Shield Plan holders can also purchase insurance riders that provide additional complementary coverage; these riders usually provide first-dollar coverage with either a yearly deductible or zero copayment. Premiums for riders cannot be paid with MediSave.
In recent years, there have been sharper increases in Integrated Shield premiums, especially for riders with no copayment, a trend largely reflective of increases in private hospital insurance claims. 20 To address concerns about the overuse of services and about overcharging, the Ministry of Health has required that new Integrated Shield Plan riders have a minimum 5 percent copayment with an annual cap on copayments. 21
There are also private insurance options, offered by for-profit insurers, that are not integrated with MediShield Life. Premiums for these other insurance options cannot be paid from MediSave. Many employers also extend medical benefits to their employees.
Because of the many insurance options available, there may be varying degrees of coverage duplication by MediShield Life, employer benefits, and personal health insurance.
Services covered: Services covered under MediShield Life are 22 :
MediShield Life does not cover cosmetic surgery or maternity charges (including cesarean sections), with the exception of treatments for serious complications related to pregnancy and childbirth.
The maximum amount that can be claimed from MediShield Life depends on the claim limit, which varies by type of treatment and length of hospital stay. The maximum claim limit per policy year is set at SGD 100,000 (USD 73,000); there is no lifetime limit.
Singaporeans are expected to pay for the rest of their health care costs (after government subsidies and MediShield Life payments) from their MediSave accounts or out-of-pocket. MediSave can be used to pay for many services, including chronic care, maternity care, fertility treatments, hospice and palliative care, and day rehabilitation services.
Limits on withdrawals from MediSave accounts ensure that Singaporeans have enough in those accounts for basic health care needs in old age. Withdrawal limits are adequate to ensure that most charges incurred for outpatient treatments and treatments at subsidized inpatient wards are covered. Withdrawal limits have been raised to keep pace with rising costs.
Cost-sharing and out-of-pocket spending: Under MediShield Life, residents have an annual deductible of SGD 1,500 to SGD 3,000 (USD 1,095–2,190) and coinsurance of 3 percent to 10 percent (with the coinsurance percentage decreasing as the claimable amount increases). 23 For current outpatient treatments, there is 10 percent coinsurance.
Copayments (see table below) have been an integral feature of Singapore’s health care system as a way to retain individual responsibility for one’s health, as well as provider and system discipline pertaining to health care costs. Patients pay directly for part of the cost of services, and pay more when they demand a higher level of services. 24
Safety nets: The combination of government subsidies, MediShield Life, and MediSave has enabled seven in 10 subsidized bills to be fully paid without any cash outlay by the patient. Of the remaining 30 percent of bills, one-third require a patient payment of SGD 100 (USD 73) or less in cash, and another third cost patients SGD 100 to SGD 500 (USD 73–365). 25
MediFund is an endowment fund set up by the government in 1993 that serves as a safety net for Singaporeans who need further help with the remaining cash component of their health care bills at public health care institutions, after insurance and MediSave. MediFund coverage has been enhanced over the years to cover more outpatient and community-based care as well as to provide more targeted assistance to disadvantaged children and elderly people.
During years of budget surpluses, the government tops up the principal sum, redistributing the benefits of economic growth to Singaporeans in need. This measure has enabled an increase in enrollment in MediFund, which provided about SGD 150 million (USD 110 million) in assistance in 2017, up from SGD 4.7 million (USD 3.4 million) in 1993. 26
Physician education and workforce: Singapore has three medical schools, all of which are part of public universities. Clinical teaching is carried out almost exclusively in public health care institutions. The government regulates the number of doctors by varying the number of admissions to medical schools according to projected needs. The pipeline of doctors is supplemented by foreign-trained doctors. The government regulates the entry of these doctors by adjusting a list of approved overseas medical schools. 28
Between 2012 and 2018, the total annual admissions of medical students to the three local universities increased by about 40 percent. Tuition fees are heavily subsidized: net annual fees for Singapore nationals are about SGD 29,000 to 33,000 (USD 21,000 to 24,000) for five-year undergraduate medical programs, or SGD 47,000 (USD 34,000) for four-year graduate programs. 29 Upon graduation, all medical students are required to work in the public health care system for four to five years. 30
As of 2018, Singapore had 13,766 registered medical practitioners, with nearly two-thirds in the public sector. This translates to about 2.4 doctors per 1,000 people, a significant increase from 1.9 in 2012. Around 41 percent of doctors are specialists. 31
Primary care: Primary care is provided through public polyclinics and private GPs. There are currently 20 polyclinics and more than 2,200 GP clinics. 32 Polyclinics usually have more than 10 doctors and some also provide dental, psychiatric, and allied health services. Polyclinics provide 20 percent of primary care, with a strong focus on chronic-disease management. 33
The majority of GP clinics operate as solo practices (including those run by clinic chains), and primarily operate on a fee-for-service payment model; the clinics have flexibility to set their own fees. Patients can choose a primary care doctor at a polyclinic or at a GP clinic, and they can usually walk in and be seen the same day without needing a prior appointment. Patients are free to change providers or to be seen by two or more providers over a given period.
The Ministry of Health has launched several initiatives over the years to tap into the capability and capacity of GPs, including the Chronic Disease Management Program, which covers 20 chronic diseases. Another initiative, the Primary Care Networks (PCN) scheme, aims to anchor effective chronic-disease management in primary care through the organization of like-minded GPs in a network. As of 2019, there are 10 primary care networks and more than 350 participating GP clinics. The ministry provides resources to these PCNs for managing patients with complex needs, including nurse counsellors and care coordinators, chronic-disease registries, and administrative support. In return, GPs in PCNs are expected to adhere to stipulated clinical quality requirements. 34
In terms of manpower, 59 percent of registered doctors are nonspecialists, including primary care doctors and those still undergoing specialist training in public institutions. The gross median monthly income for GPs is SGD 13,707 (USD 10,006), while the gross median monthly income for specialists is SGD 20,078–23,705 (USD 14,657–17,305). 35
Outpatient specialist care: Specialist outpatient services are provided by both the public and the private sector on a fee-for-service basis. Public-sector specialists are salaried and see both private and subsidized patients in the specialist outpatient clinics of public hospitals and national specialty care centers. 36 Fees for private and subsidized patients at these clinics are determined by and paid to the hospital.
Polyclinic referrals are considered subsidized patients at specialist outpatient clinics, while referrals from GPs are treated as private patients unless they are referred by clinics accredited by the Community Health Assist Scheme. Patients who refer themselves to specialist outpatient clinics are considered private patients. Private patients can choose their specialist, while subsidized patients have a specialist assigned to them.
Private specialist clinics receive referrals from GPs as well as self-referrals, and have flexibility to set their fees.
Administrative mechanisms for direct patient payments to providers: Singaporeans prepay for care through MediSave (via payroll deductions) and MediShield Life (mandatory premiums).
After-hours care: Polyclinics are not open at night or on Sundays and public holidays. However, a significant number of GP clinics are open at night and on weekends and public holidays. Thirty GP clinics are open 24 hours, as are emergency departments in public hospitals and some emergency clinics in private hospitals. There are also telehealth providers that are available any time of day.
Hospitals: As of 2017, Singapore had 18 acute care hospitals: nine public hospitals, eight for-profit hospitals, and one not-for-profit Catholic hospital.
In total, Singapore has 2.4 beds per 1,000 population. 37 The majority of public-hospital patients are admitted through emergency departments, making up more than 70 percent of admissions. Admissions to private hospitals tend to be elective.
Legally speaking, public hospitals are corporatized companies wholly owned by the government. 38 As owner, the government can shape hospitals’ behavior without having to resort to onerous regulations or purchase negotiations. 39 This has enabled the Ministry of Health to reorganize the public health care system to ensure better-coordinated and seamless care (for example, by creating integrated clusters of public hospitals and polyclinics).
The government funds public hospitals on the basis of diagnosis-related groups (DRGs) for inpatient and day surgery services and per piece rates for outpatient visits subject to an overall block. 40 Public hospitals are required to meet expenses from government payments and patient fees. Public hospitals are allowed to keep surpluses but need to meet shortfalls from their reserves, unless there are exceptional circumstances.
The government introduced community hospitals to provide rehabilitation and subacute care, including to patients who have dementia or need palliative care. Community hospitals also provide outpatient services, such as day rehabilitation. There were seven community hospitals in 2018, with nearly 1,700 beds. 41 The Ministry of Health pays community hospitals on a per-diem basis. Patients admitted to community hospitals may be eligible for subsidized care, ranging from 20 percent to 75 percent based on their per-capita household income and residency status.
Mental health care: The Institute of Mental Health, a public hospital, is Singapore’s only psychiatric hospital, and provides acute tertiary psychiatric, rehabilitative, and counselling services for children, adolescents, adults, and the elderly. It has both inpatient wards, with more than 2,000 beds, and Specialist Outpatient Clinics at various community locations. The Community Mental Health Team, which comprises doctors, community psychiatric nurses, and allied health professionals, provides community-based treatment and psychosocial rehabilitation for patients after discharge so they may continue to live in the community while working toward recovery.
Other public and private hospitals also have psychological medicine departments or specialists that offer psychiatric services.
The Ministry of Health is working with health care institutions and professionals to implement the Community Mental Health Plan, which was launched in 2017. By early 2019, mental health or dementia services were available at 12 polyclinics.
The ministry has also expanded the Mental Health General Practitioner (GP) Partnership program to encourage patients with emotional health issues to seek early treatment. GPs in the program can prescribe psychiatric drugs at a lower cost and have a liaison coordinator to facilitate referrals between services. Patients can also get subsidies for mental health conditions.
The number of GPs trained to diagnose and support persons with mental health conditions grew from 70 in 2012 to 190 by the end of 2018. These GPs are supported by 20 community intervention teams led by allied health professionals. 42
Long-term care and social supports: There are three main groups of long-term care services.
Center-based services. These cater to seniors who require care services during the day on a regular basis while their family members are at work. As of 2017, there were 102 day care centers, dementia day care centers, day rehabilitation centers, and senior care centers.
Home-based services. As of 2017, there were 21 home medical and home nursing providers, and nine home palliative care providers. 43 In addition, three inpatient hospices are run by charitable organizations.
Long-term residential facilities. Nursing homes provide a range of services, including medical care, nursing care, and rehabilitative services to residents who are unable to be cared for at home. Respite care is also available at some of the nursing homes. As of 2017, there were 73 nursing homes, including private, nonprofit, and public facilities, contributing a total of approximately 14,900 beds. 44 The Ministry of Health contributes to the growth and development of eldercare services in Singapore, as well as the development of nursing homes, under its Build Own Lease framework.
MediSave cannot currently be used for nursing home services or home-/center-based services, but residents can use ElderShield, a basic long-term care insurance scheme designed to cover severe disability, especially during old age, on top of government subsidies of up to 80 percent for various services. 45 Coverage is automatically extended to all citizens and permanent residents with a MediSave account when they reach age 40. Residents can opt out, and the opt-out rate is 5 percent in recent years. 46
ElderShield is a prefunded insurance scheme within which premiums are collected during policyholders’ working years and risk-pooled within each generation. Premiums do not rise with age, and policyholders are covered for life. The scheme provides monthly cash payouts of $400 for 72 months or $300 for 60 months, depending on the plan. 47 Policyholders can also purchase supplements that provide higher coverage — for example, higher payouts or a longer duration of payouts — and pay for premiums using their MediSave coverage (up to a limit).
The Ministry of Health’s key legislative tool for regulating health care providers is the Private Hospitals and Medical Clinics Act. Health care facilities, such as hospitals, nursing homes, clinics, and clinical laboratories, are required to obtain a license before they can commence operations. They are also subject to regular compliance audits and relicensing.
Health care professionals are regulated by their respective professional boards, which are set up as statutory bodies under the Ministry of Health. In addition, hospitals are required to put in place a clinical privileging system that grants doctors the appropriate scope of practice commensurate with their areas of competence. There are also additional requirements for specific high-risk specialized procedures or services; doctors are required to apply for authorization before providing these procedures or services. Hospitals must establish quality assurance committees to monitor and evaluate the safety and quality of their practices, procedures, and services.
The ministry benchmarks the performance of Singapore’s system against international counterparts, and conducts annual patient experience surveys of public health care institutions. Some health care institutions have voluntarily undertaken external accreditations, such as those provided by the Joint Commission International.
Under the Chronic Disease Management Program, participating primary care clinics and medical institutions are expected to provide care in line with the latest clinical practice guidelines or best available evidence-based practice, as well as to track clinical data to monitor outcomes. 48 Participation is a prerequisite for joining the Community Health Assist Scheme. 49
In public hospitals, care is provided based on patients’ clinical condition, rather than on their subsidy status. When nonsubsidized drugs or treatments are deemed clinically required and cannot be replaced by subsidized alternatives, needy patients receive assistance (such as through MediFund) in accessing these drugs or treatments.
Singapore has also adopted a system of differentiated charges, based on a patient’s and his or her family’s ability to pay. Means-testing is used, but even higher-income patients receive subsidies when they access subsidized services (although they pay more than lower-income patients). For example, higher-income patients who choose to stay in subsidized C-class hospital wards will receive up to a 65 percent subsidy while lower-income patients in these wards receive up to an 80 percent subsidy. Nearly all government-funded services, from acute to long-term care, have differentiated charges, except for polyclinic services and accident and emergency services.
The government has also introduced schemes to assist specific cohorts of Singaporeans:
In 2018, the Ministry of Health established three integrated clusters organized by geographic regions and made up of public-sector institutions ranging from acute hospitals to polyclinics. Each cluster is expected to develop and strengthen partnerships with GPs and other community partners across care settings to enable seamless care transitions and also to anchor care more firmly in primary and community settings.
The clusters have embarked on several programs, ranging from preventive health and chronic disease to caring for frail patients. The clusters also work with social and other related agencies to support residents who have varying combinations of health and social needs as well as to address social determinants of health. While the elderly remain a key area of focus, the clusters have adopted a life-course approach and are progressively addressing other age groups as well.
In addition to ensuring better system integration, the reorganization of providers seeks to derive greater economies of scale, to facilitate scaling up of programs and services, and to tap into a larger pool of manpower resources and talents.
Since 2011, Singapore’s national electronic health record (EHR) has been progressively deployed to both public and private health care institutions to support the goal of “One Patient, One Health Record.” The national EHR is owned by the Ministry of Health and managed by Integrated Health Information Services. The secure system collects summary patient health records from different health care providers, and authorized health care professionals can access the EHR to have a holistic and longitudinal view of a patient’s health care history. 54 As of 2019, more than 1,300 health care institutions participate in the national EHR. 55
Singaporeans and permanent residents can access some of their health records via HealthHub, a national one-stop health portal. They can also track and manage their medical appointments, request medication refills or renewals, and view bills and make payments at select public hospitals, national centers, and polyclinics. 56
The hallmark of Singapore’s health care market has been strong government control and oversight. 57 Demand- and supply-side controls encourage patients and providers to be judicious and cost-conscious in their use of health care services. 58 In addition, the public sector’s role as the dominant health care provider sets the benchmark for the private sector, as well as the entire health system’s ethos of deemphasizing profit maximization. 59,60 Private providers need to ensure that they do not price themselves out of a market where public-sector care is available, and therefore offer reasonable prices and quality.
The corporatization of public hospitals has introduced commercial accounting systems, which provide a more accurate picture of operating costs and instill greater financial discipline and accountability. In the costing and funding of hospitals, the depreciation of equipment and other fixed asset costs are registered and factored into annual budgets and, in turn, patient charges and government funding.
The Ministry of Health also closely monitors cost-recovery ratios for different types of services to ensure that public hospitals’ overall revenue is not excessive. Costs and funding rates are set through a detailed costing exercise. Funding amounts are then incremented annually, taking into consideration volume and cost growth, but set deliberately lower than actual trends. This process compels hospitals to be disciplined with their spending, as they have limited ability to charge patients more to recover any shortfalls. 61
The Ministry of Health encourages the appropriate use of drugs through the provision of subsidies for essential drugs. Patients pay only a small amount for clinically relevant and cost-effective drugs on the standard drug list. Subsidies are also available for a list of more expensive, nonstandard drugs under the Medication Assistance Fund. Patients receiving these drugs must meet predefined clinical criteria. The Medication Assistance Fund scheme was expanded in 2012 to allow each institution to determine, through a specific set of guidelines and a peer-review mechanism, whether a nonstandard drug should be subsidized by the fund. 62
The Ministry of Health publishes public and private hospitals’ history of transacted hospital bill amounts and operation fees to encourage consumers to be price-conscious and to stimulate price competition among providers. In late 2018, the ministry also began setting fee benchmarks for private-sector health professionals, with input from an independent committee that includes representatives from the medical community, providers, patients, and payers. Intended to help the public assess the reasonableness of provider charges, the benchmarks will be reviewed and updated regularly, with reference to historical data. Doctors are not prohibited from charging lower or higher fees. 63
Other cost-control initiatives include using technology to improve productivity, and the use of group purchasing procurement to obtain better prices. Supply chain professionals from the three public health care clusters harness their synergies in meeting procurement and supply chain needs. Public hospitals are also evolving their model of care to help Singaporeans receive care in the most appropriate setting.
In late 2017, the Ministry of Health launched its Beyond Healthcare 2020 strategy to move more care to the community, encourage health promotion, and ensure value. 64
In 2018, the ministry launched the Licensing Experimentation and Adaptation Program, a regulatory “sandbox” for identifying and understanding new health care innovations, such as telemedicine and mobile medicine, through industry partnerships. The program seeks to develop an appropriate regulatory approach to facilitate such innovations while prioritizing patient safety and welfare. 65
To provide better protection against long-term care costs, the ministry will launch CareShield Life in 2020 to replace ElderShield. The new scheme will have higher cash payouts, starting at SGD 600 (USD 438) and increasing over time. There is no cap on payout for as long as the policyholder remains severely disabled. 66 CareShield Life will be mandatory for citizens and permanent residents born in or after 1980. In addition, people with severe disabilities can withdraw up to SGD 2,400 (USD 1,752) per year, or SGD 200 (USD 146) per month, from their own and their spouse’s MediSave account for their long-term care needs, after setting aside a minimum amount for other health care needs.
The Ministry of Health will also be launching ElderFund in 2020, to provide discretionary assistance, up to SGD 250 (USD 183) per month, for severely disabled and needy citizens who require further help with their long-term care costs.
In addition, the ministry and public hospitals are working on value-driven outcomes with inter- and intra-hospital benchmarking to minimize unnecessary variation and to encourage the adoption of best practices. The ministry has also started to bundle payments to facilitate care transformation and reward efficiency. And it has implemented a pay-for-performance framework to reward the three public health care clusters that do well on key priorities, such as reducing hospital-acquired infections, managing length of stay, and minimizing waiting time for specialist appointments.
The author would like to acknowledge Chang Liu and Ruru Ping of ACCESS Health International as contributing authors to earlier versions of this profile.