

While most Americans have focused on the Covid-19 pandemic, the nation’s other great epidemic has continued to burn. Drug overdoses now claim the lives of over 100,000 Americans every year, a rate that appears likely to continue or grow for the foreseeable future. While the crisis once was concentrated predominantly in rural, white communities, the introduction of novel synthetic opioids, particularly fentanyl, into the illicit drug supply has spread overdoses across urbanizations.
Today, small-town and big-city leaders alike desperately need tools to fight back against the drug crisis. It can often seem as though drug policy is outside the ambit of local leaders, who lack the capacity to go after international traffickers or spend trillions of dollars on care. But local government, as the closest entity to the front lines of the crisis, plays a vital role in addressing it.
This paper, therefore, explores options for local policymakers to respond to the drug crisis. In particular, it considers six frequently discussed local-scale policies:
For each policy, this paper examines the evidence, offers estimates of costs, and provides caution where necessary. The overall goal is to give local policymakers a better understanding of what tools they have to more effectively tackle the other health crisis in their communities.
Between 2000 and 2021, the annual drug overdose (OD) death rate in the U.S. quadrupled, to roughly 107,000 deaths by the end of last year.[1] Drug overdose deaths now routinely exceed those from homicide, suicide, car crashes, and many medical causes.[2] By best estimates, the drug OD death rate is now six times higher than its highest point in the 20th century[3] and well above any point since the initiation of the modern drug-control regime.[4]
Public perception of this crisis lagged behind its growth. About 20 years ago, drug OD deaths were rising disproportionately among white, middle-aged Americans in predominantly rural or small metropolitan areas, particularly in Appalachia and the upper Midwest, areas particularly affected by the decline in manufacturing employment. As depicted in books like J. D. Vance’s Hillbilly Elegy or Beth Macy’s Dopesick, the white, rural drug crisis is often thought to combine longstanding socioeconomic disenfranchisement with the acute effects of predatory pharmaceutical firms, which flooded communities with highly potent prescription opioids and created iatrogenic (physician-caused) addiction.
While this picture remains accurate in some regards, it is also incomplete. Figure 1 breaks out OD death rates by level of urbanization for three years: 2000, 2010, and 2020.[5] The percentages over the 2010 and 2020 bars represent the percent increase in the OD death rate compared to the same urbanization in the prior decade.
Figure 1
Drug Overdose Death Rates in 2000, 2010, and 2020, by County Urbanization

As of the year 2000—near the beginning of the crisis—OD deaths were more common in more urban counties, that is, those that contained large or medium-sized cities or large cities’ suburbs (“large fringe metro”),[6] and less common in small cities, towns, and rural (“NonCore [Nonmetro]”) counties. Over the next 10 years, OD death rates rose across urbanizations, but they rose more—as captured by the percent change—in less urban areas. The total effect was that by 2010, OD death rates were higher in more rural areas than they were in more urban ones, particularly in the most rural counties—creating the impression of the crisis as a predominantly rural problem.
But between 2010 and 2020, the pattern again reversed. Although all urbanization types saw a large increase in OD death rates, the increases this time were largest for cities. Although the drug crisis continued to worsen in rural areas, the increases in OD deaths in cities were so extreme that cities overtook rural areas and again had the highest death rates.[7]
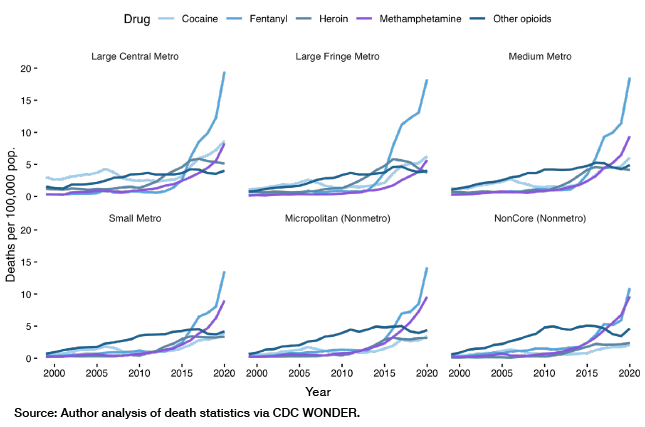
Figure 2 shows OD death rates by year, urbanization, and type of drug involved. This chart shows in clearer detail the phenomenon captured in Figure 1. In particular, it shows how precipitously from 2000–10 OD deaths rose in small-town and rural America, driven primarily by prescription opioids (included in “other opioids” in the CDC’s system). Then, between 2010 and 2020, illegally manufactured fentanyl (IMF) and other novel synthetic opioids arrived on the scene, eclipsing death rates from other types of drugs. This is particularly true in large and medium cities, where illegal opioids (formerly heroin, now also IMF) are a far larger problem than methamphetamine, which is a bigger issue relative to IMF for more rural Americans.[8]
Figure 2
Drug Overdose Death Rates 1999–2020, by Type and Urbanization

These data illustrate what drug policy scholar Daniel Ciccarone has called the “triple wave” epidemic.[9] A first iatrogenic wave was caused by the widespread distribution, diversion, and consumption of prescription opioids, particularly Purdue Pharmaceutica’s OxyContin.[10] Policymakers responded to this wave through pressure on pharmaceutical firms and tighter controls on prescription opioids. Those now-dependent individuals responded by switching from prescription opioids to heroin, igniting the second “wave” driven by heroin deaths.[11]
The third wave was ushered in by drug suppliers introducing synthetic opioids into the drug supply. This shift was the product of a variety of factors: the acquisition of relevant chemistry knowledge by Mexican drug trafficking organizations, China’s production of fentanyl, and then, later, grey-market precursor chemicals.[12] Synthetic opioids are, from a producer’s perspective, a vastly superior product: easier and much cheaper to produce and transport, as well as more potent and therefore more compact.
Whereas the second wave stemmed from people with an opioid-use disorder joining an (existing) illegal market, the third wave was instigated by the producers. As one RAND analysis notes, “dealers are not transparent when it comes to the distribution of synthetic opioids, using them to adulterate heroin or pressing them into tablets made to look like prescription medications.”[13] Unlike the iatrogenic wave, there is no reason to believe that fentanyl has drawn in many more users. Rather, the wave of deaths comes from increasing the death rate of a preexisting stock of users.[14] In fact, users are often alarmed by the introduction of far more potent fentanyl into their supply of illegal opioids (that had previously been mostly heroin).[15]
Many other drugs are now adulterated with IMF. Such multidrug combinations are increasingly common and particularly dangerous. Drug deaths regularly involve multiple substances, with the simultaneous presence of opioids and cocaine, methamphetamine, benzodiazepines, or alcohol leading to death.[16] Figure 3 shows drug OD death rates, distinguishing between deaths that did and did not involve synthetic opioids.
Figure 3
Drug Overdose Death Rates 1999–2020, by Urbanization and Synthetic Involvement
This figure recapitulates Figure 2, insofar as IMF is a bigger share of the problem in large and medium-sized cities than it is in small cities and rural areas. Absent IMF-involved deaths, for example, the OD death rate in more urban areas would be below its 2016 peak; in less urban areas, it would be at or above it. But Figure 3 underscores that IMF in isolation is not the problem. Rather, it is IMF leaching into the urban drug supply more generally, which can cause people with histories of (comparatively) less harmful use to experience deadly overdoses.[17]
Drug policy interfaces uncomfortably with America’s federalized system. Drug selling, consumption, addiction, and death play out at the local level, but supply is driven by forces at the national and international scale—high-level, wholesale distribution organizations that span state borders, the international drug market and border enforcement, and the socioeconomic factors that marginally affect the tendency to produce and consume drugs, among others. It may be easy for local policymakers to feel like the drug crisis is simply too big a problem for them to cope with, and that only national or international action can stem the tide.
While drug policy must be conducted at all levels of government, there is a significant role for local leaders to play in combatting the crisis. In this section, I discuss policy approaches uniquely suited for the local level.
Naloxone Access/Distribution
Naloxone is an FDA-approved medication that can rapidly reverse the effects of opioid overdose by binding to opioid receptors without causing the respiratory depression and other harmful effects of opioids that lead to overdose.[18] Because of these potent properties, naloxone is a powerful lifesaving tool. Many jurisdictions already equip first responders with naloxone, while some have experimented with wider distribution, including to people at risk of OD or to the general public.
But does such distribution have a significant impact on overdose death rates? In allocating scarce dollars, is naloxone a good use of money? And to whom should naloxone be distributed?
One view is that widespread naloxone availability will uniformly reduce overdose deaths by increasing the probability that the drug will be available at the time of overdose. Some argue, however, that this effect could be counterbalanced by “moral hazard”—by reducing the risk associated with each individual use, greater naloxone access may lead to more use, cancelling out beneficial effects or actually leading to more overdose deaths. It is also the case that having a naloxone supply is not necessarily enough: just because naloxone is available does not mean that people will use it.
One way to understand the effect of naloxone availability on OD deaths is to look at research on “naloxone access laws” (NALs). Such laws make naloxone more available, for example, by allowing the purchase of naloxone with or without prescription, or preventing prescribers or bystanders from being held liable for administering naloxone to someone other than the person to whom it was prescribed or in the process of a criminal act (i.e., consuming drugs).[19] What is the impact? A comprehensive review of studies on NALs finds that the passage of NALs is generally associated with either no effect on or a decrease in opioid overdose mortality.[20]
Not all NALs are the same, however, and different laws may have different effects. Of the studies covered by the aforementioned review, one found that NALs immunizing prescribers from liability reduced OD deaths by 23%, while other NALs had no impact.[21] Another found that removing criminal liability for possession of naloxone was associated with a 16% reduction in overdose mortality.[22] And a third found that the only NAL with an impact contained provisions that allowed pharmacists to dispense naloxone directly, reducing OD deaths by 34%.[23] Lastly, one paper found no effects of NALs except for laws permitting civilians to administer naloxone, which was associated with a significant increase in OD deaths.[24] Why so much ambiguity? One possible answer is that naloxone-access laws tend to go into effect at the same time, often across many locales, which means there is little variation to exploit for purposes of identifying their effect. There may be effects that we can’t easily measure.
What should policymakers take away from this (confusing) evidence? One safe conclusion is that there is little evidence that NALs, with the possible exception of lay administration laws, lead to an increase in OD deaths, and at least some evidence that they reduce them. Another reasonable inference is based on the insight that NALs expand access to people other than first responders. If there is some evidence that giving naloxone to the man on the street can reduce OD deaths, it stands to reason that trained responders equipped with naloxone are very likely to reduce deaths.
Another way to think about naloxone is in terms of costs and benefits. Naloxone is relatively cheap—usually somewhere around $20 to $50 per dose for the generic form and up to $150 per dose for name-brand Narcan.[25] That cost is almost always worth it, insofar as naloxone is rarely going to be used in a situation where the harm it prevents is worth less—for example, in terms of quality-adjusted life-years—than the cost of using it. There may be individuals on the margins for whom naloxone use is harmful, but it’s likely that in most individual instances, it is beneficial.
Local policymakers, then, should certainly support giving their first responders—EMTs, firefighters, and police officers—naloxone. In addition, distributing naloxone to the average person on the street, and even the average person who uses drugs, is as at least unlikely to do net harm, and quite possibly, it may have a net benefit. Policymakers worried about the risk of “moral hazard” should think about how to minimize downside without losing the upside of naloxone distribution. Distribution could be tied to offers of treatment, for example, and repeated emergency department visits as a sign that someone may need more intensive attention. Fitting naloxone into the matrix of other drug treatment and control methods, in other words, may help to mitigate any risks associated with it while preserving its benefits.
Invest in Treatment Capacity
Drug treatment is a dramatically underutilized resource. The federal Substance Abuse and Mental Health Services Administration (SAMHSA), a division of the Department of Health and Human Services, estimated that as of 2020, some 40.3 million Americans needed treatment for a substance-use disorder (SUD), including about 18.4 million suffering from an illicit drug–use disorder, and 4.2 million suffering from a substance-use disorder related to an illicit drug other than marijuana. By comparison, only about 4 million Americans actually received treatment, roughly two-thirds of whom were in treatment for a drug-use disorder (many in addition to an alcohol-use disorder).[26]
One explanation for this “treatment gap”—sometimes the only explanation offered—is inadequate funding of treatment. But some of the gap also reflects disinterest on the part of users. Some disagree with the premise that they need treatment—SAMHSA’s definition of a SUD is quite broad, and denial is a hallmark of addiction. Yet even among people who said they needed treatment, only one in five actually made an effort to get it.[27] In other words, even among those who believe they would benefit from drug treatment, many are not actually getting into treatment.
Of course, there are many barriers to getting someone into treatment: health insurance, stigma, lack of childcare, etc. And not all drug treatment is created equal—some approaches are far more efficacious than others (a full review is beyond the scope of this paper, but the issue is treated briefly below). That acknowledged, it is worthwhile for municipal policymakers to ask holistically whether they have adequate capacity to meet the demand for drug treatment, and whether they are successfully connecting those who want help with the help that they need.
Local government has a role to play in treatment access. As of 2020, local, county, and community governments operated about 4% of treatment facilities—a small share but double that administered by state, federal, or tribal governments.[28] And government at all levels funds drug treatment that is provided by non- and for-profit providers.[29] In addition, local government often oversees drug treatment in jails, a place where some people get access to treatment while others lose it, thereby increasing their risk of an overdose. Government can also play a role in advertising for drug treatment and connecting people with substance-use disorders to treatment through the social services system, criminal justice system, and street outreach.
Treatment for substance-abuse disorders is not bulletproof. The National Institute of Drug Abuse estimates a 40 to 60% relapse rate, which NIDA attributes to a failure to understand treatment as an ongoing, rather than one-time, intervention.[30] On the other hand, much treatment depends on therapeutic approaches, from cognitive behavioral therapy to contingency management. In the case of opioid-use disorders, however, several medications—buprenorphine, methadone, and naltrexone—exist to effectively substitute for harmful opioids, mitigating cravings without leading to respiratory depression and death. Such “medication assisted treatment” has been shown to substantially reduce overdose mortality.[31] Although local government cannot necessarily set regulations about the use of “medication assisted treatment,” it can in many cases encourage or even mandate its use in treatment facilities or jails it oversees, funds, or operates.
Cost estimates for treatment will necessarily vary based on the kind of treatment. NIDA estimates, for example, that methadone maintenance costs roughly $4,700 per year per patient; somewhat older estimates (vintage 2001–02) peg the cost of outpatient treatment at between $1,500 and $8,200 per patient per year, though these may have changed.[32] Those costs can be balanced against their benefits: analysis usually indicates that the social benefits yielded by drug treatment are worth the cost, with one commonly cited estimate being seven dollars saved to one dollar spent.[33] This comes from reduced health harms as well as reduced social harms, as expanding substance abuse treatment also reduces crime in the surrounding area, for example.[34] But they can also be balanced against alternatives: as mentioned below, the cost of methadone maintenance therapy is similar to the cost of supervised consumption.
Limited as it is, treatment is often the only way to mitigate the long-run risks and harms of disordered drug use. Filling the “treatment gap” is not innovative, but it is lifesaving, and local leaders should ask if they have done so before trying other, more daring, approaches.
Drug Courts
Many people with substance-abuse disorders interact with the criminal justice system, either because they are apprehended for drug possession/distribution, because of behavior driven by their SUD (for instance, theft or public disorder), or simply incidentally, that is, they both offend and have a SUD. In many jurisdictions today, some of these people are diverted from the regular criminal justice process of trial, conviction, and incarceration to specialized courts meant to target the “root cause” of their behavior, namely their drug abuse. Such courts usually offer enrollees (“clients”) an opportunity to have their sentences reduced or waived altogether, assuming they complete a course of drug treatment actively overseen by the court, including through regular check-ins and the dispensing of rewards and punishments. The model depends, in essence, on a carrot-and-stick approach: if a client gets clean, he stays out of jail; if he fails, he gets locked up.[35]
The first drug court opened in 1989 in Miami-Dade, Florida, in response to the crack cocaine epidemic.[36] As of 2014, there were over 3,000 drug courts nationwide, serving an estimated 127,000 participants. That number of drug courts represents a 24% increase over 2009, meaning almost certainly that even more exist today. As of 2014, drug courts cost an average of $6,008 per participant, though the range of reported costs extended from $1,200 to $17,000, and much data was missing.[37]
Drug courts appear to have a significant effect on clients’ tendency to reoffend—a proxy for both their drug use and the harmful effects of their drug use on their communities. Multiple meta-analyses find that drug courts reduce enrollees’ recidivism rates by between 9 and 24%, albeit with substantial heterogeneity in the effectiveness of different kinds of drug courts.[38] These effects persist for at least three years after leaving the program, with one study finding effects up to 14 years later.[39] A 23-site study confirmed that drug court involvement not only reduced criminal behavior but also actual criminal drug use.[40] These findings suggest drug courts are a winning option for local executives who want to reduce crime while being compassionate.
Depending on the laws within their jurisdiction, local administrators have the power to establish drug court programs. This is in part because many judges are locally elected, and successful drug court programs require a committed judge to spearhead the effort. But it is also because a successful drug court program requires coordinating many resources—access to treatment, housing, jail capacity, etc.—across multiple local government agencies. Such coordination requires local administrative competency to get it done, and so local executives should see doing it as partially their responsibility.
Wastewater Tracking
In spite of the scale of the drug overdose crisis, the U.S. continues to struggle with tracking drug overdose and use in real time. The elimination of previous surveillance systems, namely the Drug Abuse Warning Network (DAWN) and Arrestee Drug Abuse Monitoring (ADAM) programs, have effectively blinded policymakers at a time when up-to-date information is essential.[41] The CDC does, as of recently, report provisional and partial estimates of monthly OD deaths on a one-month lag. Local coroners can track deaths, and local emergency departments can track nonfatal overdoses, but a death or overdose is the outcome we want to avoid. Policymakers at all levels of government need tools for tracking drug use in real time, so as to enable a proactive response before drugs kill.
One solution is to track the level of drug metabolites—the excreted byproduct of metabolizing a given substance—in municipal wastewater. Wastewater testing has been shown to be an effective indicator for nearly two decades, and it has been used to compare drug consumption rates in major European cities.[42] Australia has conducted a nationwide drug wastewater surveillance program since 2016, and as of 2021 was monitoring the consumption of 12 substances across 58 waste-treatment sites covering 57% of the population.[43] It is in many ways preferable to surveys, as it can be tracked day-to-day and avoids social desirability bias—people can lie, but pee can’t.
The information derived from wastewater surveillance can be used for a variety of purposes. It can, according to one review of the approach, “monitor temporal and spatial trends in drug use at different scales, provide updated estimates of drug use, and identify changing habits and the use of new substances.”[44] Because it can tell authorities what drugs are being used, and where, in real time, it allows the targeting of relevant resources—law enforcement, social services, treatment, etc.—both to the areas where they are most needed and with the tools they most need (naloxone, e.g., is more useful in the case of a surging opioid OD than a methamphetamine OD). The great boon of wastewater surveillance is that it allows real-time response to trends, precisely what is missing from many locales’ toolboxes.
Wastewater surveillance is particularly attractive because it is universally identified as cost-effective method of gathering information compared to more conventional approaches.[45] The European Monitoring Center for Drugs and Drugs Addiction estimates the cost of analysis as between €100 and €200 (roughly $105 to $210) per sample, where a sample represents many, many people—the number of people contributing to a waste treatment site could be tens of thousands or more.[46] Comparisons from other wastewater-based epidemiology approaches are instructive: wastewater monitoring of alcohol, nicotine, and caffeine consumption reduced costs from roughly $127 per person (the cost of a conventional questionnaire) to $0.58 per person, a 200-fold reduction.[47] A World Bank analysis pegs the cost of wastewater surveillance for Covid to between $0.20 and $3 per person per year.[48]
The U.S. has lagged far behind in this area, but some cities are now using wastewater testing to track the Covid-19 pandemic, working with the CDC under the auspices of the National Wastewater Surveillance System.[49] Wastewater testing allows cities like Boston and Minneapolis to project a rise in Covid cases before they impact hospitals;[50] wastewater testing for drugs can produce similar ahead-of-the-curve information. In fact, the infrastructure already in place for Covid-19 testing should lower the start-up cost of adding wastewater testing to the fight against opioids.
Supervised Consumption Sites
A number of major cities across the U.S.—including New York, Seattle, and Philadelphia—have opened or attempted to open “supervised consumption sites” (SCSs) within their jurisdictions.[51] Such venues, sometimes also called “safe consumption sites” or “overdose prevention centers,” offer a place for people to use drugs under supervision—usually by medical professionals—who can administer oxygen, naloxone, or other lifesaving support as necessary. Although officially sanctioned SCSs are new to the U.S., they have a long history in other countries, with over 120 sites operating in Australia, Canada, and across Europe. Unsanctioned SCSs have operated in the U.S. since at least 2014.[52]
Proponents of SCSs argue that they reduce drug-related harms for existing users, both because they make it easier for people using drugs to access overdose-reversing medication and because they can connect those same people to sterile use equipment (needles, pipes, etc.) and treatment. Critics, meanwhile, argue that they normalize drug use, may only delay overdose deaths (since most SCS clients continue to also use outside of SCSs) without necessarily leading to cessation of drug use, all while contributing to crime, disorder, and drug consumption in the broader community. They also note that SCSs supervise only a small share of use sessions—about 5% of use sessions in Vancouver in the early 2000s, for example.[53] That small share of use sessions is likely concentrated among the most risk-avoidant (and therefore least overdose-prone) users, mitigating the claimed benefits.
The total evidence, in either direction, is best characterized as both lacking and somewhat mixed. Research focuses disproportionately on just two SCSs (one in Vancouver and one in Sydney), which may not be representative. One RAND Corporation review of the literature notes that most of the studies on SCSs—especially those which underpin estimates of their cost-effectiveness—“ merely report associations that do not permit causal inference.” They offer, for example, evidence that safe drug use—sanitary practices, for example—is positively correlated with frequency of visits to Vancouver’s SCSs. This association could mean that SCS attendance drives safer use, but it could also mean that those who are prone to safer use anyway are also more likely to go to SCSs.[54] Such problems limit what we can conclude about SCSs’ effects in general.
Several studies do offer quasi-experimental measures of the effects of SCSs. Two studies based on the SCS established in Sydney, Australia, find that it reduced opioid-related calls for ambulance service relative to the rest of New South Wales but not a reduction in actual overdose deaths.[55] Another, based on Vancouver, identified a reduction in overdose mortality in the half kilometer around the SCS relative to the rest of the city.[56] The causal literature also finds no adverse effects on crime and few adverse effects except possibly on public disorder.[57]
There are issues, however, about which the literature does not speak. It is particularly hard to isolate the general effect of SCSs on the intensity and extent of drug use. Use at SCSs may delay, rather than accelerate, transition to treatment, increasing the cumulative lifetime risk of overdose death outside of the facility.[58] And tacit social sanction of drug use, even in the name of harm reduction, may shift potential users’ willingness to start using at the margin. There has also not been much attention in the literature to a SCS’s possible effects on neighbors, including effects on their sense of safety or property values.
These concerns are speculative, of course. But negative social effects from SCSs have been documented. A 2020 review by the government of Alberta found that the seven SCSs the province had opened since 2018 were associated with an increase in drug OD deaths, drug-involved aggressive behavior, crime, and debris in their immediate vicinity. The committee responsible for the review noted that, “Except for Edmonton, stakeholder feedback predominantly suggested that the SCSs have had a negative social and economic impact on the community. In Edmonton, however, there were reports that stakeholders felt intimidated and were prevented from expressing their true sentiments and opinions about these sites out of fear of retribution from site supporters.”[59]
SCSs are also probably illegal under the “Crack House Statute” of the federal Anti-Drug Abuse Act (ADAA) of 1986, which makes it unlawful to “knowingly open, lease, rent, use, or maintain any place, whether permanently or temporarily, for the purpose of manufacturing, distributing, or using any controlled substance.”[60] Advocates argue that that prohibition does not apply when a “third-party visitor” acts with criminal intent, and that the original intent of the ADAA did not include the regulation of “public health facilities.”[61] But federal courts sided against Philadelphia’s SCS, which made that argument in its legal dispute with the Department of Justice.[62] The Biden administration has signaled that it may not interfere with more recent city experiments with SCSs, although such a stance is likely to change from administration to administration.[63]
Should these issues scare policymakers off from setting up SCSs? Bracketing the question of legality, not necessarily. The scale and urgency of the drug crisis may mean that radical policy solutions are the appropriate way forward. At the same time, there is much we do not know about the true impact of SCSs—they may have positive impacts, no impact, or negative impacts. And they may or may not be the best use of scarce dollars.
As ever, it is worth weighing costs against benefits. Most cost-benefit analyses focus on Vancouver’s InSite SCS, which cost between $2 and $3 million (Canadian) per year in 2007 dollars, including about $1.5 million for the supervised injection component of its services (i.e., not counting counseling, primary health care, or other services).[64] That amounts to an annual operating cost of between $2 and $3.1 million (U.S.) in today’s dollars, including about $1.5 million in the cost of providing supervised consumption services.65[65] Is this cost worth it? It depends on how one thinks about it. As the RAND report notes, “supervising all injections for someone who uses twice a day could cost approximately Can$5500–7300 per year. That might be in the same range as the cost of providing methadone for a year to a patient in the United States.” Whether a SCS or treatment is a better use of the marginal dollar is a matter of municipal priority.
If a municipality does opt to set up a SCS, it should first and foremost prioritize rigorous evaluation of its impact. That should include both quantitative metrics—overdose-related deaths and ER admissions, drug-associated and not-associated crime, even measures of disposed needles—and qualitative ones, including regular surveys of all relevant stakeholders, including neighbors. If individual people cannot be pseudo-randomly assigned to access the SCS, then policy evaluators should at least predesignate “treatment” and “control” areas of the city that are substantively similar on observable qualities and measure how the introduction of the SCS affects the aforementioned metrics.
In other words, policymakers should understand any foray into SCS not so much as a guarantee of success as an experiment. Experimentation may be warranted, but it should be regarded with the sober caution that experimental policymaking demands.
Drug Market Interventions
Much of drug control policy works either by reducing demand—discouraging people from initiating drug use or helping them desist—or by reducing the harms of drug use. Supply-side approaches are the province of law enforcement: the interdiction of drugs and the cash it generates, and the arrest and incarceration of those who benefit, from street-level dealers up to kingpins.
A longstanding question in drug policy is how, or if, these policies can be effective. On the one hand, it is likely that policing can reduce the criminal behavior incidental to and often overlapping with drug use or sales. But it’s less clear how effective law enforcement is at controlling supply. Arresting low-level dealers or sweeping up even tons of drugs is just a drop in the bucket of the massive international drug market. The rise of synthetic drugs likely exacerbates this problem because the dramatic cost-savings they have brought makes it harder for supply reduction to drive up the price and thus reduce use.[66] This is a particular challenge for local administrators, who lack the reach or capacity to bring down international drug smuggling rings, a task usually reserved to the DEA. Local cops can often feel like arresting drug dealers and users is little more than an exercise in catch-and-release.[67]
In recent years, however, there has been promising evidence in favor of another supply-side approach, the “Drug Market Intervention” or “Initiative” (DMI). The approach applies policing methods of “focused deterrence” or “pulling levers,” which entail targeting the small number of offenders who drive the majority of crime in a given area.[68] DMIs target areas with high concentrations of active drug sales, the “drug markets” that crop up in many American cities and are a significant contributor to OD deaths, at least as measured by spatial concentration.[69] During a DMI, a police department will identify drug dealers in a target area, build cases against them, then execute a “call in,” in which offenders are rounded up and notified that they can either get out of the drug game—with the support of the city’s arrayed social services—or go to prison.[70] Doing so creates a clear and powerful disincentive for offenders to continue to deal, a deterrent far more certain than the often random arrests under the conventional approach.
The earliest DMI was set up in High Point, North Carolina, in 2004. It initially targeted a large drug market in the city’s West End neighborhood, then expanded to three other drug markets. During implementation, “overt drug activity … was almost entirely eliminated,” with no displacement of drug activity to other areas. Violent crime also fell, driven by the areas where the drug markets were.[71]
Since then, a number of other jurisdictions have created their own DMIs, with varying levels of success. Successful implementations have been identified in Rockford, Illinois, and Nashville, Tennessee.[72] But a DMI in Peoria, Illinois, did not have a significant impact.[73] And in a seven-site study of implementation, just four had any actual call-in meetings, and only one successfully reduced crime overall.[74]
This last finding, the authors note, reflects the challenges of following the original High Point model successfully: “The DMI program was challenging for sites to implement and resulted in significant reductions in crime in the site with the implementation fidelity that was highest and most similar to the original site.”[75] Indeed, implementing a DMI is more complicated than doing standard drug busts. They entail coordination across government, including the police department, state/district/county attorneys, social services providers, mayors or other executive’s offices, and, ideally, civil society actors like nonprofits and churches. They can also be costly: a study of DMIs implemented in two cities suggested they cost police departments on the order of $100,000 to $150,000 per intervention.[76]
That said, the cost and risk of failure should be balanced against current approaches to local-level interdiction, which are often of limited efficacy. Particularly given the scale of the crisis, any jurisdiction willing to consider radical harm-reduction interventions (e.g., SCSs) should also be willing to consider a DMI.
Thanks in large part to miraculous medical innovation, Covid-19 is now far less a threat to life today than it was two years ago. But as one epidemic recedes, another continues. Unlike Covid, there is no sign of the drug crisis abating: it is likely that, at current rates, drugs will eventually kill more people cumulatively than Covid did in its first three years. There does not appear to be any vaccine or any virus-destroying medication coming.
But while the current scale of death is unprecedented, there are steps that government, particularly local government, can take to stem the tide. Naloxone distribution, treatment capacity, and drug courts are all effective tools for reducing death and minimizing the harms of drug use. Wastewater surveillance, long an underappreciated tool in the U.S., is primed for expansion thanks to its use during the pandemic. More experimental approaches like SCSs or DMIs are also worth investigating, assuming local leaders do so with an eye to their harms, benefits, and cost.
The drug crisis is not the rural problem it was 10 years ago. It is now, more so than ever, everyone’s battle. Local leaders are on the front lines of this conflict—it is incumbent on them, therefore, to act.
Charles Fain Lehman is a fellow at the Manhattan Institute for Policy Research, working primarily on the Policing and Public Safety Initiative, and a contributing editor of City Journal. He has addressed public safety policy before the House of Representatives, at universities including Cornell and Carnegie Mellon, and in the Wall Street Journal, Dallas Morning News, New York Post, National Review, and elsewhere. He was previously a staff writer with the Washington Free Beacon, where he covered domestic policy from a data-driven perspective. Lehman graduated from Yale in 2016 with a BA in history.
The Manhattan Institute thanks the Klinsky Leadership Series for its support in the publication of this paper.
Are you interested in supporting the Manhattan Institute’s public-interest research and journalism? As a 501(c)(3) nonprofit, donations in support of MI and its scholars’ work are fully tax-deductible as provided by law (EIN #13-2912529).